-
Patricia Stathatou authoredPatricia Stathatou authored
Waste PPE: addressing the challenge
Framing: PPE waste generation and footprint
Patricia
Waste generation
- Landfill volumes have fallen due to the lockdown, whereas medical waste from hospitals have been significantly increased due to the disposal of tons of soiled PPE.
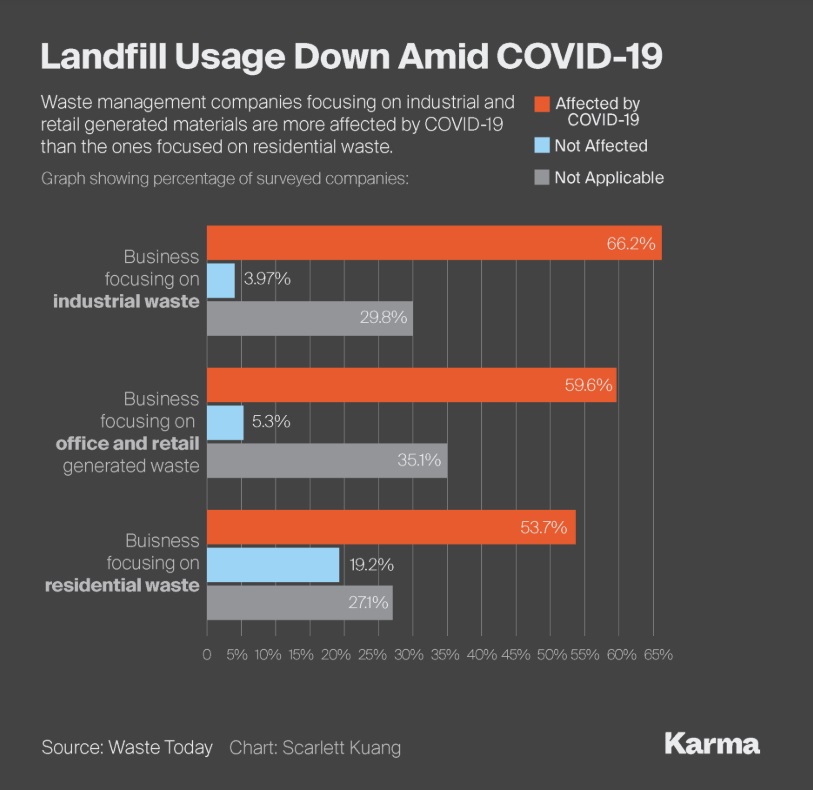
- Reduction in landfill volumes during the pandemic (survey from mid-March to mid-April - Lodge, 2020)
- Inbound materials from offices and retail operations have fallen by more than half.
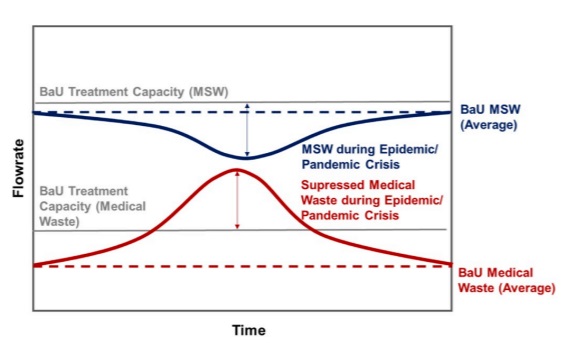
- Figure 2: The expected trend of medical and MSW waste flow during the pandemic (Klemes et al., 2020)
- China has the most data on this issue:
- Amount of MSW in large and medium cities was reduced by 30% during the disease outbreak.
- However, the generation of medical waste increased sharply - by 370% in Hubei Province, with a high proportion of plastics.
- 20 January-31 March: The accumulated medical waste in all China was estimated as 207 kt.
- In Wuhan, medical waste increased from the normal level of 40 t/d to about a peak of 240 t/d, exceeding the maximum incineration capacity of 49 t/d.
- US data on medical waste generation:
- Stericycle is the largest hauler of regulated medical waste in the US & operator of 50 medical waste treatment plants. The publicly traded, Illinois-based company neither owns landfills nor recycles equipment.
- Stericycle CEO Cindy Miller said on May 7 that the company has seen "a small decrease" in medical waste volumes "due to the postponement of preventative care and elective surgeries and the temporary closure of smaller, independent health care practices."
- IBISWorld reports on PPE Manufacturing Statistics in the US cost ~$1,000.
- Contact Stericycle?
- Contact MGH, through Lorena Altamirano?
- Contact other major players in waste management, such as Waste Management Inc. and Republic Services Inc?
- Other suggestions?
Waste management & footprint
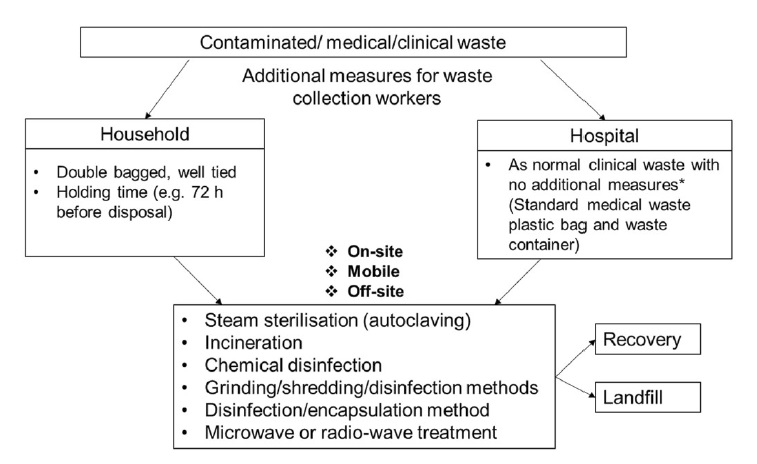
- Effective management of biomedical & healthcare waste requires appropriate identification, collection, separation, storage, transportation, treatment/disinfection and disposal/recovery.
- Figure 3: The main waste handling approaches for contaminated waste during COVID-19 (Klemes et al., 2020)
- Incineration and steam sterilisation are the most common pathways for thermal treatment of hazardous medical waste.
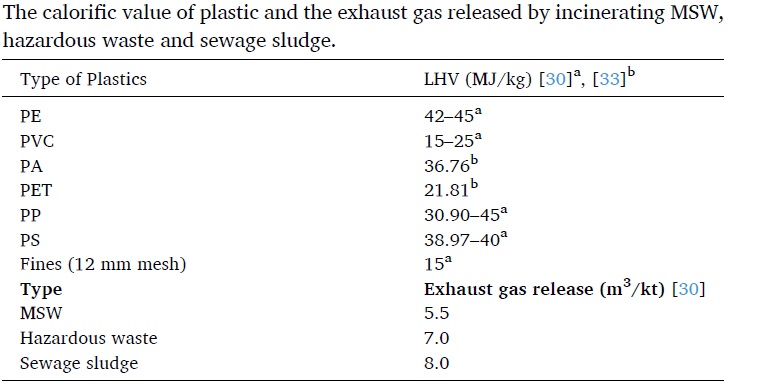
- Plastics have calorific values comparable to conventional fuels (Gasoline: 43 / LNG: 47 MJ/kg).
- Figure 4: The calorific value of plastic and the exhaust gas released by incinerating MSW, hazardous waste and sewage sludge (Klemes et al., 2020).
- The energy embodied in plastic waste can be recovered if adequately managed.
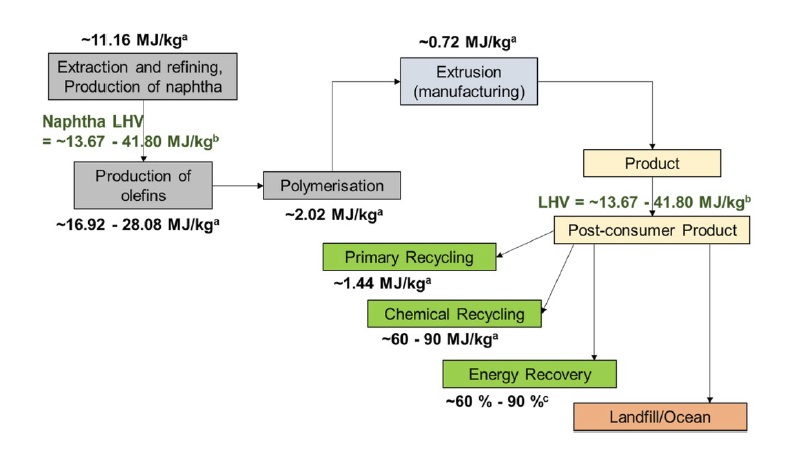
- Figure 5 shows the typical energy consumption in the life cycle of plastic products (withouth considering the transportation stage).
- The embodied energy in the plastic can be recovered through primary and mechanical recycling, energy recovery and possibly chemical recycling (depolymerisation). The energy required for
- The concept of Plastic Waste Footprint (PWF) can be used as a metric for environmental burdens, to compare alternative solutions on plastic production & waste management: the total mass of plastic waste generated by a process/product or service minus the amount of plastic avoided /reused / recycled / reprocessed.
- Further research:
- Collect data on PPE Lifecycle: CO2/GHG emissions of PPE generation & waste management
Nik
- Stericycle Earnings Report indicates no increase in April compared to previous year, expects major surge post June 1 as America opens.
- Wuhan produced 40 tons per day pre-coronavirus, 240 tonnes per day during peak coronavirus. Could expect a 6 fold increase. Rapidly built waste treatment plants. - Multiple medical waste experts told Waste Dive the virus is classified as a Category B situation, and so exposure to it poses a lower risk threshold than Ebola or another Category A disease.
- 3 days surface expectancy, Source: https://www.nejm.org/doi/full/10.1056/NEJMc2004973
Overview Reuse: priority (use cycles); then eventually recycle/degrade/incinerate
Interventions: tech
- Sorting tech
- Materials (reusable, e.g. face shield)
- Evaluation of resuse/recycle approach vs business as usual
- Evaluation of quality of PPE (e.g. light sensor for opacity, whether its scratched up)
- Storage solution
- Cleaning (autoclave or other)
- Distribution tech, 'sharing' approaches as a collective, e.g. sharing PPE, sharing autoclave access; large and small clinics (Fab Labs could be a distribution Hub)
- Recycling or degredation or incineration
- Technologies that prolong the life of PPE (e.g. face shield cleaner)
- Developing new PPE from recycled feedstock - enabler: Material characterization technology; ASTM standards
Interventions: institutional
- Protocols for storing
- Fab Labs help with recycling PPE that has been stored for an adequate time period
General approaches
- Reusable PPE
- Recyclable PPE
- Biodegradable PPE > Self-deteriorating?
Reusable reusable PPE can reduce waste if PPE is made from materials that can be autoclaved. Increasing access to autoclaves is something that the Fab Lab network may be able to play a role in, with the most promising decentralized technology being stovetop and solar autoclaves. In addition, making reusable PPE from materials that can be autoclaved would also be a key intervention. Would appreciate other's input and feedback in developing this further.
Current approach to PPE disposal Used Covid-19 PPE is most often classified as infectious, which means a disposal method needs to prevent further disease transmission. At present, there are two approved methods for disposal: incineration and autoclaving (Corse et al. 2015): Incineration destroys the virus with high temperatures. Hazardous waste is often disposed of in this way, and in developed countries, waste incineration plants are used for energy generation (creating some positive environmental value); however, 'lock-in' of waste streams is an issue (i.e. waste is required to supply these plants when alternative pathways such as recycling could be viable and more effective overall from a sustainability standpoint). Also, toxic gases and GHGs are released, although these can be scrubbed (Fletcher 2020). Autoclaving is the more interesting choice from a circular economy perspective: autoclaves use high temperature and pressure to kill viruses and other pathogens on surgical instruments (common usage) and other PPE (potential). "High temperatures in the autoclave disrupt membranes and denature proteins and nucleic acids in transmissible agents such as spores, bacteria, and viruses. Autoclaves work by creating a vacuum to replace all initial air with steam that directly interacts with the material" (Eurotherm, 2014, cited in Corse et al. 2015). Autoclaves in theory could be used to sterilize reusable PPE.
Challenges with autoclaving:
- Many hospitals do not have autoclaves on-site, relying on third party contractors (Waste360).
- Autoclaves can be expensive, making them prohibitive investments
- Autoclaves come in different sizes, making some models more/less appropriate for different materials. e.g. in the Ebola crisis, large autoclaves were needed to disinfect mattresses of patients
- Autoclaves can only handle the following types of materials: Pyrex or Type I borosilicate glass, polypropylene, polycarbonate, gloves, stainless steel, pipette tips, paper (put inside autoclave bags), and media solutions. They are not compatible with organic solvents, poorly heat resistant plastic such as polystyrene, polyethylene, and metals excluding stainless-steel (Jove 2020).